Scorched Skin - Prehospital Burn ManagementComment on this page
Original article → Scorched Skin: A Guide to Prehospital Burn Management
Author(s): David Hostler, PhD, NREMT P, DMT A
Published April 6, 2015 | Journal of Emergency Medical Services
Burns are common in the United States, and more than 450,000 require medical treatment each year. Many of these burns are severe and more than half of cases admitted to the hospital require treatment at a burn center.1 Although an EMS provider will rarely encounter a serious burn injury, the initial assessment and treatment can influence patient outcomes, which require providers to remain knowledgeable on current treatment modalities.
All Burns Are Not the Same
Intact human skin is an amazing barrier that protects us from the environment, aids in thermoregulation and prevents dehydration. Unfortunately, the skin is easily damaged when exposed to high heat and flame. Cutaneous pain receptors are activated at 100–113 degrees F (37.7–45.0 degrees C). A 50-degree F increase will result in third-degree burns and irreversible damage to the skin and underlying tissues. Fundamentally, all burns damage the skin and some portion of the underlying tissues. However, there are important mechanistic differences among the various types of burns that may influence treatment decisions.
Thermal burns are the most common type of burn and are the result of skin exposure to scalding water, open flame or intense heat. This type of burn represents more than 80% of the cases treated in the U.S.2 The tissues are physically damaged, destroying the skin barrier. Injury thickness will vary depending on the duration and the intensity of the exposure. Destruction of the skin challenges the thermoregulatory system and patients may become hypothermic if care isn’t taken to prevent heat loss. These patients may also require aggressive airway management, fluid resuscitation and pain management.
Chemical burns can result from accidental or intentional exposure to thousands of different chemical compounds. Chemicals capable of burning the skin are broadly categorized into acids (compounds with pH < 7), alkalis or bases (compounds with pH > 7), and organics. Acid burns form a scab in the wound (coagulation necrosis) and tend to be self-limiting. Alkali burns are more severe because the burning process (liquefactive necrosis) doesn’t scab over, which results in deeper burns. Organic compounds, including gasoline and kerosene, damage the skin by destroying the fat in the cell membranes. For all chemical burns, the extent of the injury is proportional to the concentration of the chemical, the duration of the exposure and the volume of agent on the victim.
Acid, alkali and organic skin burns all have similar initial treatment pathways. Given the progressive nature of cutaneous chemical burns, removing contaminated clothing and jewelry is the first step in decontamination and will limit the exposure. Providers should use proper personal protective equipment to protect themselves and dispose of contaminated articles appropriately. Brush any powders from the skin and immediately begin to flush the contaminated areas with plain water. Ideally, irrigation should continue during transport but providers should be cautious about causing hypothermia when irrigating large skin surfaces. Increasing the air temperature in the ambulance during transport and using warm water for irrigation will help prevent loss of body heat.
Chemical burns to the eye should be flushed with normal saline. Placing a Morgan lens over the globe may facilitate this process. Topical ophthalmic analgesics, such as tetracaine eye drops, may facilitate the placement of the Morgan lens and reduce discomfort for the patient during treatment. Never attempt to neutralize a burn (e.g., treat an acid burn with a base or vice versa). The neutralization process will create additional heat and worsen the injury.
The severity of electrical burns is difficult to accurately assess in the prehospital setting. The electrical current passes through the body, making it difficult to know what tissues have been affected. Depending on the path of the electrical arc, these burns can result in significant internal injuries while leaving little evidence on the skin surface.
Both alternating and direct current (AC and DC) sources can cause an electrical burn. Assuming one source is safer than the other may lead to careless practice when working around electricity and can result in serious injury or death. Lightning is the most extreme form of DC current. This high-voltage injury can depolarize the entire heart, resulting in asystole and temporarily inactivate the respiratory center of the brain, causing respiratory arrest.
Electric current passes through the body between two or more points of contact. The severity of the injury will worsen with longer exposure to the electrical source. The points of contact themselves may appear to be minor, possibly looking like small punctures surrounded by blackened skin. However, high-voltage currents may cause large lesions at the points of contact. Current conducted through the body will depolarize the muscle cells causing muscle spasms and contractures. When a threshold stimulus is exceeded, victims may be unable to release themselves if one of the points of contact is the hand. Both AC and DC currents can cause respiratory arrest and fatal cardiac arrhythmias. Other mechanisms of injury occasionally seen with electrical injuries are arc flashes (current passing through the air), which may cause skin burns or ignite clothing, and thermal contact burns caused by an electrical current heating metal objects (e.g., jewelry) worn by the victim.
Patient Assessment
Providers should take steps to protect themselves from injury. Qualified responders wearing the appropriate protective garments and respiratory protection should remove chemical burn victims from the exposure site. Electrical sources should be turned off at the source.
Cutaneous burn injuries are visually distracting, making it difficult for providers to concentrate on the initial assessment— especially if the burn is complicated by other traumatic injuries. The airway should be assessed immediately and steps taken to secure the airway if the provider suspects there’s thermal or chemical damage that may cause the airway to swell. Challenges to ventilation include smoke/steam inhalation and circumferential or near-circumferential burns around the chest. These chest burns prevent expansion of the rib cage during inhalation and must be treated in the ED by making incisions through the skin, called an escharotomy, to expose the fatty layer beneath the burn, which allows the chest to expand.
Document the circulatory status (heart rate and blood pressure) and Glascow Coma Score (GCS) during the initial and continuing assessments. Serial assessment will document the course of the burn injury and the patient’s responsiveness to resuscitation. Once exposing the patients for a secondary survey, take immediate action to prevent body heat loss.
It’s important to document the circumstances surrounding the burn injury. Thermal burns resulting from structure fires may be complicated by inhalational injuries. If the victim’s clothes caught fire, note the type of clothing. Natural fibers such as cotton and wool burn while most manmade fibers melt and complicate cutaneous burns. For chemical burns, document the chemical agent and, if known, the concentration and volume of the chemical. When treating patients suffering from an electrical injury, document the type of current and the voltage of the electrical source.
Burn Assessment
After the initial treatment and secondary survey, the provider should rapidly determine the extent and severity of the burn. When the burn is caused by a single source, such as an open flame, the skin directly exposed will be most severely burned while areas of skin further from the source will be less severely injured.
The extent of a burn injury is reported as the total burn surface area (TBSA). This number represents the percentage of the total skin surface covered by the burn. The “rule of nines” is typically taught to EMS providers to estimate burn size. The rule is based on certain areas of the patient’s body representing approximately 9%, or a multiple of 9%, of the skin surface area. Alternatively, the size of the patient’s hand, including the fingers, represents approximately 1% of that patient’s body surface and can be used to estimate the size of irregularly shaped burns.
Burn depth in the field can be somewhat subjective, but there are hallmarks to help the provider differentiate between partial thickness (first- and second-degree) and full thickness (third- and fourth-degree) burns. First-degree burns are limited to the outermost layer of skin (epidermis). They’re red in color and hypersensitive to pain. These burns rarely require medical treatment and shouldn’t be included in the TBSA calculation. Second-degree burns involve the epidermis and some portion of the dermis. These burns tend to blister. They’ll appear pink and wet and blanch when touched.
Third-degree burns destroy the epidermis and the entire dermal layer. These appear whitish or charred and won’t blanch when touched. Destruction of the nerve endings in the burn area causes the burn itself to be painless. These burns will require extensive surgical excision and grafting and will heal with significant scars. The fourth-degree burn also damages the underlying muscle, connective tissue and possibly the bone, and often results in amputation.
Cooling Burns
Cooling thermal burns and decontaminating chemical burns should be part of initial prehospital care. There are many benefits to cooling the burn site, including reduced burn depth and more rapid healing. Aggressive cooling of burns, however, can also result in hypothermia, which is associated with high mortality among patients treated at a burn center. One study examined a statewide trauma registry that included more than 12,000 patients treated at a burn center.3,4 Arriving at the center with a temperature below 36.5 degrees C was independently associated with death. Every 0.5 degree C below that threshold temperature increased the risk of mortality 1.91 times, even when statistically controlling for clinical confounders such as sex, age and burn size.
Avoid using room-temperature IV fluids to resuscitate burn victims, as these infusions will reduce body temperature.5
Larger burns, smaller patient body mass, trauma suffered at the same time as the burn injury and prehospital GCS < 8 are all patient factors associated with burn-related hypothermia. Not surprisingly, environmental factors associated with burn-related hypothermia include the need for extrication at the scene and burns suffered during winter months. Appreciating these patient and environmental cues when treating burn patients should remind the provider to take extra precautions to prevent loss of body heat during resuscitation.
Shock & Fluid Resuscitation
Severe shock should be expected when burns exceed one-third of the TBSA. A portion of the plasma volume enters the burn injury, resulting in hypovolemia similar to what’s seen after traumatic injury. The decreased blood volume causes tachycardia, reduced cardiac output and vasoconstriction. An important element of prehospital burn care is reestablishing the vascular volume to restore tissue perfusion and limit further injury in the areas surrounding the burn.
Burn patients should have a large bore IV catheter placed for fluid administration during transport. Providers should consider placing a second catheter for large burns (> 30% TBSA). Colloid solutions won’t be effective since capillary permeability is increased around the injured skin in the hours following the injury; crystalloid solutions are preferred.
The American Burn Association, Advanced Burn Life Support (ABLS) course recommends starting infusion rates of 500 mL per hour for patients aged 14 years and older. Children aged 6–13 years should be resuscitated at 250 mL per hour and burn victims younger than 5 years should be resuscitated at 125 mL per hour. These infusion rates can be adjusted after the volume requirements are determined.
While inadequate resuscitation leads to shock and acute renal failure, over-resuscitation can lead to excessive edema formation in the days following the injury. For adults suffering thermal and chemical burns, total fluid volume for the first 24 hours is calculated as: 2 mL crystalloid x the patients mass (kg) x the TBSA (%) of second- and third-degree burns.
For example, a 100 kg patient suffering 20% second degree-burns and 20% third-degree burns would require 8,000 mL of fluid (2 x 100 x (20 +20)) in the first 24 hours. Half of this volume (4,000 mL) is given in the first eight hours following the injury. Only 500 mL is required in the first hour (4,000 mL/8 hours), so EMS providers shouldn’t provide too much fluid in the initial phase of resuscitation. Adult burn patients suffering high-voltage injuries and pediatric burn patients may require larger fluid volumes during resuscitation.
Transport
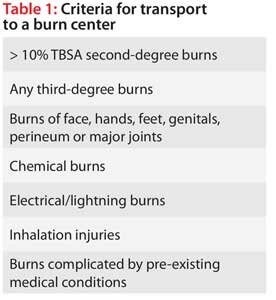
Serious burns are complex cases that require skilled medical professionals trained in burn care. Even after the initial resuscitation and hospital course, the patient will required specialized wound care and rehabilitation. Serious burn cases should be transported to an accredited burn center. (See Table 1, p. 58.) Burn victims with significant trauma should be transported initially to a trauma center to be stabilized if the traumatic injuries present a greater life threat than the burn.
Conclusion
Burn injuries are devastating wounds that can result in months of hospitalization and years of therapy before healing. Burn patients may suffer posttraumatic stress disorder, depression and other anxiety disorders for years after being released from the hospital. Effective prehospital care is an important step to enhance healing and future quality of life for burn patients. Providers should be prepared to treat these patients aggressively and appropriately, and advocate for patients to be cared for at accredited burn centers.
Rapid assessment of the burn severity, airway management, preventing hypothermia and fluid resuscitation are key goals for EMS providers treating and transporting burn patients. Continuing education courses including the ABLS course will help prepare EMS providers to treat these medically complex patients.
Author
David Hostler, PhD, NREMT-P, DMT-A, is the director of the Emergency Responder and Warfighter Performance Lab at the University at Buffalo (N.Y.). He has 28 years of experience in public safety as a firefighter, paramedic, dive medic and hazmat technician. He can be contacted at
References
- Advanced burn life support course: Provider manual. American Burn Association: Chicago, 2011.
- Herndon DN, editor: Total burn care, 4th edition. Saunders Elsevier: New York, 2012.
- Hostler D, Weaver MD, Ziembicki JA, et al. Admission temperature and survival in patients admitted to burn centers. J Burn Care Res. 2013;34(5):498–506.
- Weaver MD, Rittenberger JC, Patterson PD, et al. Risk factors for hypothermia in EMS-treated burn patients. Prehosp Emerg Care. 2014;18(3):335–341.
- Moore TM, Callaway CW, Hostler D. Core temperature cooling in healthy volunteers after rapid intravenous infusion of cold and room temperature saline solution. Ann Emerg Med. 2008;51(2):153–159.
Key Terms
Chemical burn: Tissue damage caused by exposure to a strong acid or alkali, such as phenol, creosol, mustard gas or phosphorus.
Cutaneous: Referring to the skin.
Electrical burn: Tissue damage resulting from heat of up to 5,000 degrees C generated by an electric current. The points of entrance and exit on the skin are burned, along with the muscle and subcutaneous tissues through which the current passes. Fatal cardiac arrhythmia may result.
Thermal burn: Tissue injury, usually of the skin, caused by exposure to extreme heat.
Learning Objectives
- Identify the differences between types of burns.
- Learn how to assess and treat burn patients.
- Understand how to prevent your patient from becoming hypothermic while still providing adequate fluid resuscitation and burn cooling.
Further Reading
For more information on treating burns, check out previous JEMS articles:
- Burning Breath: Assessing & treating smoke inhalation & airway burns in firefighters and civilian fire victims, by David Hostler, PhD, NREMT-P, October 2014
- Lightning Strikes: Considerations when assessing & treating patients with lightning injuries, by Scott Oglesbee, BA, NRP, CCEMT-P, May 2014
- Hot Flesh: The basics of burn management, by Chad Brocato, JD, DHSc, CFO, December 2013
- Traumatic Eye Injuries: Management principles for the prehospital setting, by Felipe Serrano, MD; Lawrence B. Stack, MD; R. Jason Thurman, MD; Lara Phillips, MD & Wesley H. Self, MD, MPH, December 2013




 Last edited 2015-11-04 21:58 UTC by
Last edited 2015-11-04 21:58 UTC by ![[Twitter]](/img/twitter_box.png)
![[RSS]](/img/rss_box.png)